
In the early days of COVID-19, the World Health Organization (WHO) and the Centers for Disease Control and Prevention warned people against using masks. They wouldn't protect people against getting the disease, those organisations said. A few months into the pandemic, there was an about turn, with masks being recommended as part of a strategy to control the spread of the disease. Currently, multiple masks are recommended.
Again, while offering a scientific brief on the mode of transmission, WHO (June 2020) commented, "Transmission of SARS-CoV-2 can occur through direct, indirect, or close contact with infected people through infected secretions... which are expelled when an infected person coughs, sneezes, talks or sings... Airborne transmission of SARS-CoV-2 can occur during medical procedures that generate aerosols." A recent study published in the Lancet suggests the opposite: "The evidence supporting airborne transmission is overwhelming and evidence supporting large droplet transmission is almost non-existent." The researchers cite work demonstrating long-range transmission of the virus between people in adjacent rooms in hotels, people who were never in each other's presence.
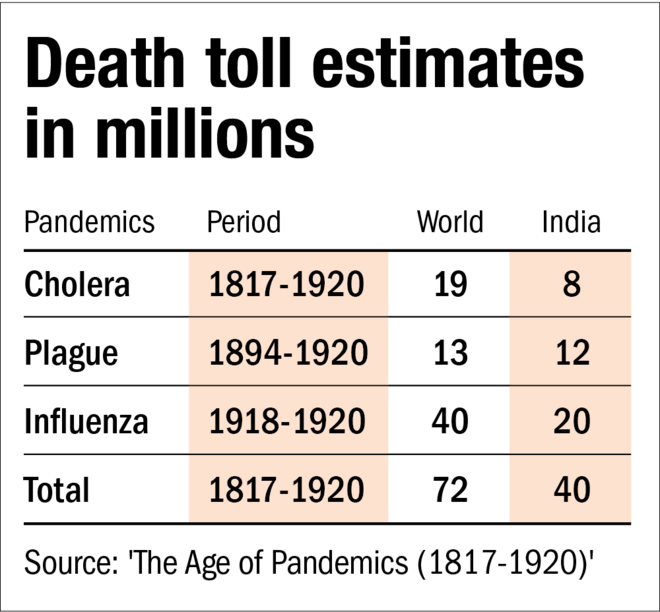
We are still some ways to go in understanding COVID-19 as a disease. In this zone of confusion, it is useful to look at the lessons history offers, and IIM Ahmedabad Professor Chinmay Tumbe's book 'The Age of Pandemics (1817-1920)' offers just such a perspective.
The three deadly pandemics
The period 1817-1920 was marked by waves of pandemics, especially in India. Asia's share of global population fell from 65 per cent to almost 50 per cent. Asia's contribution to global output fell in the same period from 50 per cent to 20 per cent.
Between 1920 and 2019, about 40 million deaths can be attributed to pandemics - the most to AIDS (30 million) but the world population has moved from two billion to seven billion. Deaths were between 1-2 per cent of population, down from over 5 per cent in the earlier century.
Cholera
Though known for centuries, a clear reference to cholera, per Prof Tumbe, appears in 1543 in Portuguese-ruled Goa. Between 1817 and 1823, the pandemic affected India, South Asia, Africa and frontiers of Europe. Robert Pollitzer, writing for the WHO, identified six pandemics starting in various years between 1817 to 1899, which could be six waves nested within one large pandemic across the century. While the first in 1817 could be said to start in Bengal, the rest likely didn't. Despite this, cholera was often referred to as 'Indian cholera'.
On the assumption that cholera was communicable by air, segregation was employed between British quarters and India settlements. Insanitary conditions at Hindu pilgrimage sites like Kumbh Mela in Haridwar and Allahabad were routinely, and wrongly, described as the reason for the disease. In England, the urban poor were disproportionately impacted - living as they were in abysmal conditions. Improvements in sewage and water supplies in Europe led to cholera receding.
Three alternate theories of the reason for the spread were prevalent - human contagion, climatic conditions, and health and hygiene. It was only in 1887 that the sanitary commissioner of Madras M C Furnell wrote, "I believe that water is the chief means by which cholera is spread, especially in India." This was at variance to the official view that it was insanitary conditions that were responsible and piped water would not make a difference.
Vaccinations developed against cholera met with public scepticism. Development of IV fluids to keep the body hydrated happened as a tool against cholera. It was finally an Indian scientist Shambhu Nath De who decoded the effect of enterotoxins on intestines.
Plague
A plague pandemic raged between 1894 to 1920. Ninety-five per cent of the lives lost were Indian, though other countries suffered as well. The connection between rat fleas and the mechanism of transfer to humans was not well understood. The initial response was a drive against insanitary conditions, with the state passing laws allowing forceable clean-up of properties, including physical search of people. This created a push-back from the population, leading to rioting and even protests against clean-ups. A common response was migration away from the centres of plague. Sometimes people would leave home and settle out in the open, in farms. Many political leaders like Tilak and Sardar Patel made their initial mark in politics by leading protests against the governmental handling of the pandemic.
Many parts of India were not infected. While initial credit was given to hygienic conditions, in the final analysis, it was the temperature at which bacteria could survive in the body of the rat flea that made the difference.
'Improvement trusts', the precursors of the Development Authorities we see in cities today, were established. The Haffkine Institute that helped manufacture vaccines for the plague led to the formation of the Serum Institute in India. Plague reduced economic growth rate of India and even China to among the lowest ever.
Influenza
Between 1918-1920, influenza struck and took the lives of 40 million humans, 50 per cent of whom were Indians. 1918 was also a year of famine in India, triggered by the third-worst drought between 1870-2000. The 1899-90 pandemic was initially known as the 'Russian flu' and its cause was attributed to 'Pfeiffer's bacillus' identified by Richard Pfeiffer. It took a while for scientists to discover that it was not the cause. It wasn't till 1930 that scientists discovered that the flu could be transmitted to pigs. This led to studies that discovered the virus but attempts to vaccinate against it were met by mutations.
The true nature of the virus that caused the pandemic in 1918 was only known in 1997. Interestingly, while the origins of the 1918 virus are still disputed, it appears to have started in Kansas in the USA. It rapidly mutated and spread to Europe, America and Africa. Undivided India had almost 5 per cent of its population affected. It received its moniker 'Spanish flu' because Spain was a neutral country in the World War and did not censor its press! Overall, the virus killed over 2 per cent of the global population.
Among the methods recommended to control the pandemic were the use of masks, avoiding crowded places and isolation for the infected persons. Lockdowns were not recommended as they "induce depression and increase the risk of catching the flu." Malnutrition increased fatalities and that was a significant contributor to deaths, especially in the United Provinces in India. Disposal of the dead was an issue.
Prof Tumbe postulates that a key reason for high deaths in India was the drought that preceded the disease. Where nutrition was adequate, mortality rates were around 4 per cent. A dislocation of the transportation system and hoarding of food grains led to food inflation that further exacerbated the problem. Industrial output suffered as well. While the economy rebounded in the next year (1919-20), economic volatility led to the emergence of new political forces, with Mahatma Gandhi taking the lead.
The decade of 1911-1921 was the only one that registered a decline in population. It also dampened death rates in the aftermath, with a large number of the susceptible having already expired. Migration both out and in was limited, given the shorter period for which the disease prevailed. Fertility that fell during the period rapidly increased later.
Why did people forget this pandemic? It was a short period in the midst of the World War and with major political upheavals in India. With no major pandemic after that, memory faded.
Pandemic lessons
History offers no clear answers to managing pandemics. As a pandemic appears, Tumbe classifies the response into four categories: denial, confusion, acceptance and erasure. He suggests that acceptance and an appropriate response can be achieved when some public memory exists of dealing with such an event. This may explain the initial better response of Kerala to the COVID crisis since it had recent experience of dealing with the 'Nipah virus' in 2018.
The cause and mechanism of the spread of a disease is often understood only years after it has first appeared. The idea of the 'super-spreader' is a myth. There is no particular pattern to the timing of pandemics. The intervention by a state depends on the accountability of the government and the push-back of its citizens. Death rates in pandemics are dependent on a wide variety of factors and management plays only one part.
Should a lockdown be implemented? While lockdowns can slow the spread of disease, they will also result in lower nutrition levels - and future deaths. Not imposing lockdowns runs the risk of high deaths and an effective lockdown due to sick people not reporting to work. Lockdowns within a country are hard to implement and can lead to migration, as was experienced in China in 1911 and in India in 2020. The choice of a shutdown cannot be left to either economists or epidemiologists as they are accountable to none and have contradictory objectives. Finally, it is a call for the political leadership to take.
Food distribution during a pandemic is possibly a good response, both as a mitigator of economic misery and a health and immunity booster to fight infection.
One of the effects of pandemics is to reduce labour availability. In the past, reduction of labourers increased their bargaining power and led to the formation of cooperatives to demand better wages. Deaths due to the disease reduced the pressure of population on land, leaving more land for the survivors. Another demographic change was the addition of women to the workforce.
Pandemics allow an opportunity for a new political leadership to emerge. Local leadership opportunities arise as rules passed by administration machinery that is overwhelmed creates problems at the micro level while implementation.
On the economic front, a sharp dip (as in 2020) is followed by an equally sharp rebound. It appears trends remain the same even as state-capacity improvements reduce the percentage of population infected.
Anand Tandon is an independent analyst








